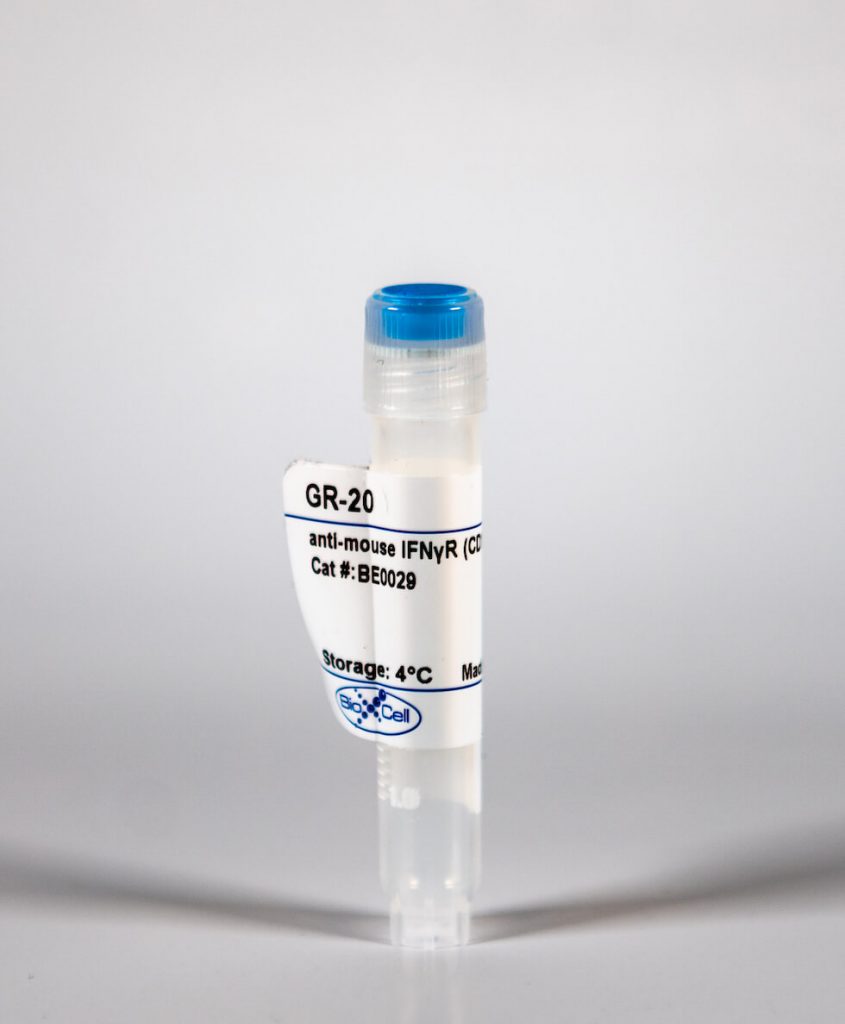
InVivoMAb anti-mouse IFNγR (CD119)
| Clone | GR-20 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Catalog # | BE0029 | ||||||||||||
| Category | InVivoMab Antibodies | ||||||||||||
| Price |
|
The GR-20 monoclonal antibody reacts with the mouse IFNγR (interferon gamma receptor) α chain also known as CD119 and IFNγ receptor 1. CD119 heterodimerizes with IFNγ receptor 2 (AF-1) to form the IFNγR, a Class II cytokine receptor. The IFNγR is expressed ubiquitously on almost all cell types with the exception of mature erythrocytes. The GR-20 antibody binds to an epitope in the ligand-binding site of the receptor and has been shown to block the binding of IFNγ to CD119 therefore inhibiting IFNγ mediated effects.
| Isotype | Rat IgG2a, κ |
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure™ pH 7.0 Dilution Buffer |
| Immunogen | BALB/c mouse monomyelocytic cell line WEHI-3 |
| Reported Applications | in vivo IFNγR neutralization |
| Formulation |
|
| Endotoxin |
|
| Purity |
|
| Sterility | 0.2 μM filtered |
| Production | Purified from tissue culture supernatant in an animal free facility |
| Purification | Protein G |
| RRID | AB_1107576 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
INVIVOMAB ANTI-MOUSE IFNGAMMAR (CD119) (CLONE: GR-20)
Folias, A. E., et al. (2014). “Aberrant innate immune activation following tissue injury impairs pancreatic regeneration.” PLoS One 9(7): e102125. PubMed
Normal tissue architecture is disrupted following injury, as resident tissue cells become damaged and immune cells are recruited to the site of injury. While injury and inflammation are critical to tissue remodeling, the inability to resolve this response can lead to the destructive complications of chronic inflammation. In the pancreas, acinar cells of the exocrine compartment respond to injury by transiently adopting characteristics of progenitor cells present during embryonic development. This process of de-differentiation creates a window where a mature and stable cell gains flexibility and is potentially permissive to changes in cellular fate. How de-differentiation can turn an acinar cell into another cell type (such as a pancreatic beta-cell), or a cell with cancerous potential (as in cases of deregulated Kras activity) is of interest to both the regenerative medicine and cancer communities. While it is known that inflammation and acinar de-differentiation increase following pancreatic injury, it remains unclear which immune cells are involved in this process. We used a combination of genetically modified mice, immunological blockade and cellular characterization to identify the immune cells that impact pancreatic regeneration in an in vivo model of pancreatitis. We identified the innate inflammatory response of macrophages and neutrophils as regulators of pancreatic regeneration. Under normal conditions, mild innate inflammation prompts a transient de-differentiation of acinar cells that readily dissipates to allow normal regeneration. However, non-resolving inflammation developed when elevated pancreatic levels of neutrophils producing interferon-gamma increased iNOS levels and the pro-inflammatory response of macrophages. Pancreatic injury improved following in vivo macrophage depletion, iNOS inhibition as well as suppression of iNOS levels in macrophages via interferon-gamma blockade, supporting the impairment in regeneration and the development of chronic inflammation arises from aberrant activation of the innate inflammatory response. Collectively these studies identify targetable inflammatory factors that can be used to influence the development of non-resolving inflammation and pancreatic regeneration following injury.