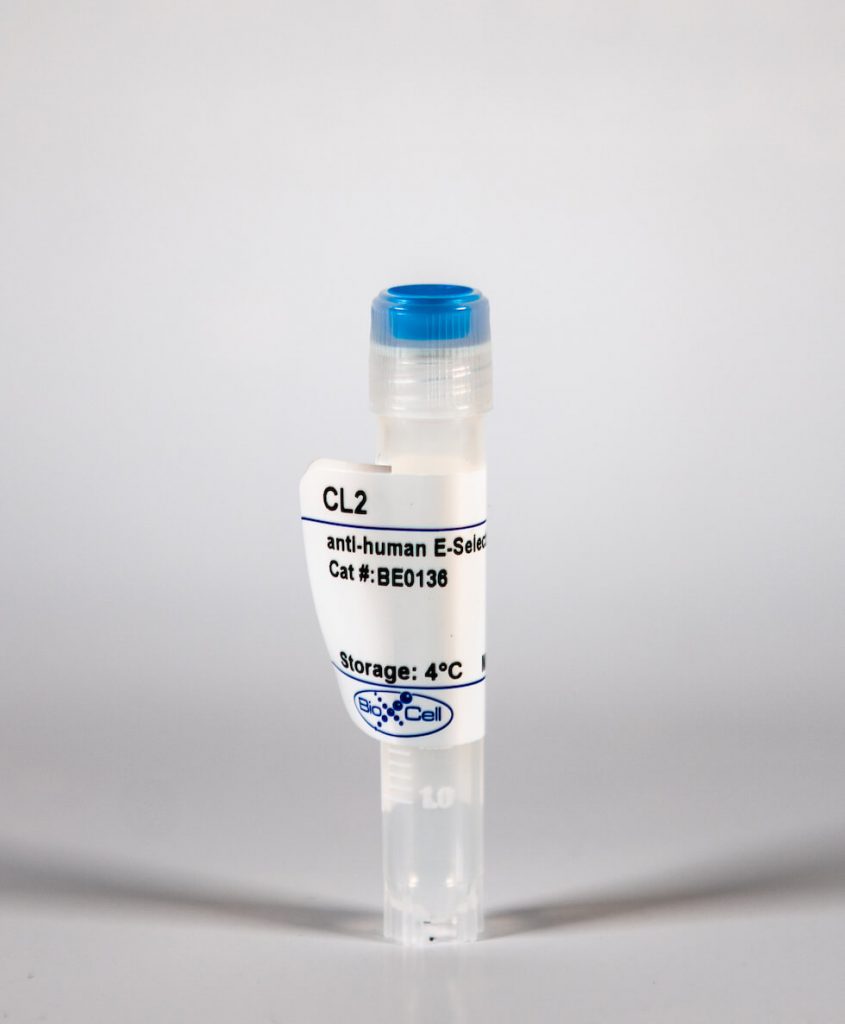
InVivoMab anti-human E-Selectin
| Clone | CL2 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Catalog # | BE0136 | ||||||||||||
| Category | InVivoMab Antibodies | ||||||||||||
| Price |
|
The CL2 monoclonal antibody reacts with human E-selectin also known as CD62E, endothelial-leukocyte adhesion molecule 1 (ELAM-1), and leukocyte-endothelial cell adhesion molecule 2 (LECAM2). E-selectin is a 115 kDa type I transmembrane protein and a member of the selectin family of adhesion molecules. E-selectin is expressed on cytokine-activated endothelial cells. Along with L-selectin and P-selectin, E-selectin mediates the initial interactions of leukocytes and platelets with endothelial cells. E-selectin is thought to play a role in inflammation, tumor metastasis, and angiogenesis. The CL2 antibody has been shown to inhibit neutrophil adhesion to E-selectin and to P-selectin.
| Isotype | Mouse IgG2a, κ |
| Recommended Isotype Control(s) | InVivoMAb mouse IgG2a isotype control, unknown specificity |
| Recommended Dilution Buffer | InVivoPure™ pH 7.0 Dilution Buffer |
| Immunogen | Not available or unknown |
| Reported Applications | Flow cytometry |
| Formulation |
|
| Endotoxin |
|
| Purity |
|
| Sterility | 0.2 μM filtered |
| Production | Purified from tissue culture supernatant in an animal free facility |
| Purification | Protein G |
| RRID | AB_10949619 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
InVivoMAb anti-human E-Selectin (Clone: CL2)
Goncharova, V., et al. (2014). “Homing of neural stem cells from the venous compartment into a brain infarct does not involve conventional interactions with vascular endothelium.” Stem Cells Transl Med 3(2): 229-240. PubMed
Human neural stem cells (hNSCs) hold great potential for treatment of a wide variety of neurodegenerative and neurotraumatic conditions. Heretofore, administration has been through intracranial injection or implantation of cells. Because neural stem cells are capable of migrating to the injured brain from the intravascular space, it seemed feasible to administer them intravenously if their ability to circumvent the blood-brain barrier was enhanced. In the present studies, we found that interactions of hNSCs in vitro on the luminal surface of human umbilical vein endothelial cells was enhanced following enforced expression of cutaneous lymphocyte antigen on cell surface moieties by incubation of hNSCs with fucosyltransferase VI and GDP-fucose (fhNSCs). Interestingly, ex vivo fucosylation of hNSCs not only did not improve the cells homing into the brain injured by stroke following intravenous administration but also increased mortality of rats compared with the nonfucosylated hNSC group. Efforts to explain these unexpected findings using a three-dimensional flow chamber device revealed that transmigration of fhNSCs (under conditions of physiological shear stress) mediated by stromal cell-derived factor 1alpha was significantly decreased compared with controls. Further analysis revealed that hNSCs poorly withstand physiological shear stress, and their ability is further decreased following fucosylation. In addition, fhNSCs demonstrated a higher frequency of cellular aggregate formation as well as a tendency for removal of fucose from the cell surface. In summary, our findings suggest that the behavior of hNSCs in circulation is different from that observed with other cell types and that, at least for stroke, intravenous administration is a suboptimal route, even when the in vitro rolling ability of hNSCs is optimized by enforced fucosylation.