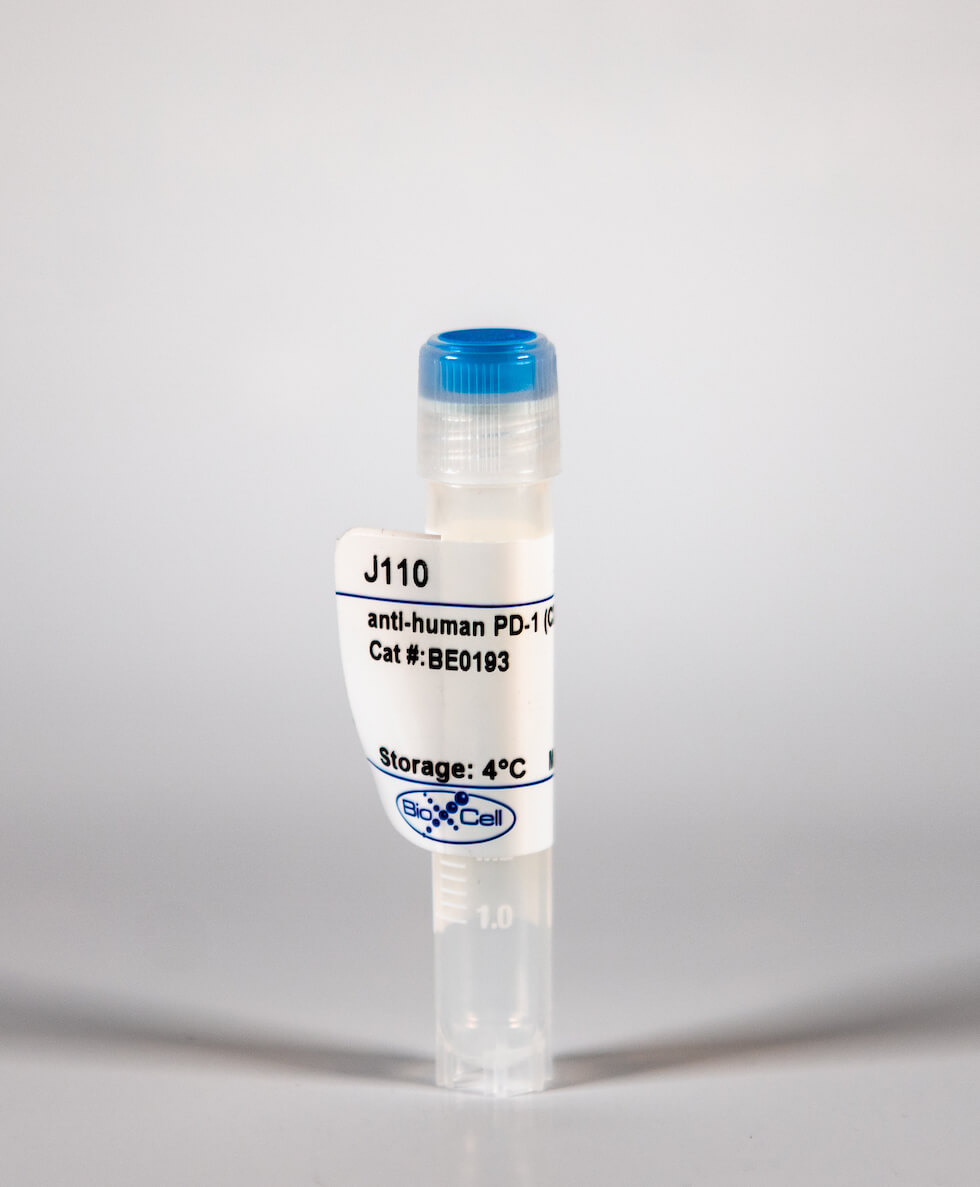
InVivoMab anti-human PD-1 (CD279)
| Clone | J110 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Catalog # | BE0193 | ||||||||||||
| Category | InVivoMab Antibodies | ||||||||||||
| Price |
|
The J110 monoclonal antibody reacts with human PD-1 (programmed death-1) also known as CD279. PD-1 is a 50-55 kDa cell surface receptor encoded by the Pdcd1 gene that belongs to the CD28 family of the Ig superfamily. PD-1 is transiently expressed on CD4 and CD8 thymocytes as well as activated T and B lymphocytes and myeloid cells. PD-1 expression declines after successful elimination of antigen. Additionally, Pdcd1 mRNA is expressed in developing B lymphocytes during the pro-B-cell stage. PD-1's structure includes a ITIM (immunoreceptor tyrosine-based inhibitory motif) suggesting that PD-1 negatively regulates TCR signals. PD-1 signals via binding its two ligands, PD-L1 and PD-L2 both members of the B7 family. Upon ligand binding, PD-1 signaling inhibits T-cell activation, leading to reduced proliferation, cytokine production, and T cell death. Additionally, PD-1 is known to play key roles in peripheral tolerance and prevention of autoimmune disease in mice as PD-1 knockout animals show dilated cardiomyopathy, splenomegaly, and loss of peripheral tolerance. Induced PD-L1 expression is common in many tumors including squamous cell carcinoma, colon adenocarcinoma, and breast adenocarcinoma. PD-L1 overexpression results in increased resistance of tumor cells to CD8 T cell mediated lysis. In mouse models of melanoma, tumor growth can be transiently arrested via treatment with antibodies which block the interaction between PD-L1 and its receptor PD-1. For these reasons anti-PD-1 mediated immunotherapies are currently being explored as cancer treatments.'
| Isotype | Mouse IgG1, κ |
| Recommended Isotype Control(s) | InVivoMAb mouse IgG1 isotype control, unknown specificity(BE0083) |
| Recommended InVivoPure Dilution Buffer | InVivoPure pH 7.0 Dilution Buffer(IP0070) |
| Immunogen | Not available or unknown |
| Reported Applications | Flow cytometry |
| Endotoxin |
|
| Purity |
|
| Formulation |
|
| Sterility | 0.2 μM filtered |
| Production | Purified from tissue culture supernatant in an animal free facility |
| Purification | Protein G |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
| RRID | AB_10950168 |
| Molecular Weight | 150 kDa |
InVivoMAb anti-human PD-1 (CD279) (Clone: J110)
Yamane, H., et al. (2015). "Programmed cell death protein 1 and programmed death-ligand 1 are expressed on the surface of some small-cell lung cancer lines." Am J Cancer Res 5(4): 1553-1557. PubMed
INTRODUCTION: Programmed cell death protein 1 (PD-1) and programmed death-ligand 1 (PD-L1) play a major role in suppressing the immune system during the formation of the PD-1/PD-L1 pathway, which transmits an inhibitory signal to reduce T cell activity. PD-L1 is often expressed in various malignant tumors. In contrast, PD-1 is generally observed in activated lymphocytes and myeloid-derived dendritic cells. Of the malignant cells, only Jurkat cells under special conditions and angioimmunoblastic T-cell lymphoma tissue cells express PD-1 on their surface. METHODS: To clarify whether the PD-1/PD-L1 pathway participates in the immunotolerance of small-cell lung cancer (SCLC) cells, we examined the expressions of PD-1 and PD-L1 on the cell surface of SCLC cell lines using flow cytometry and reverse transcription polymerase chain reaction. RESULTS: Among the four SCLC cell lines examined, only SBC-3 expressed both PD-1 and PD-L1. CONCLUSIONS: We demonstrated that both PD-1 and PD-L1 molecules were co-expressed on the surface of SCLC cells. Although the biological implications of this remain unclear, we speculate that PD-1 and its ligand on the SCLC cells may participate in the growth inhibition of tumor cells as reported in cytotoxic T cells.
Bennett, F., et al. (2003). "Program death-1 engagement upon TCR activation has distinct effects on costimulation and cytokine-driven proliferation: attenuation of ICOS, IL-4, and IL-21, but not CD28, IL-7, and IL-15 responses." J Immunol 170(2): 711-718. PubMed
The program death 1 (PD-1) receptor and its ligands, PD-1 ligand (PD-L)1 and PD-L2, define a novel regulatory pathway with potential inhibitory effects on T, B, and monocyte responses. In the present study, we show that human CD4(+) T cells express PD-1, PD-L1, and PD-L2 upon activation, and Abs to the receptor can be agonists or antagonists of the pathway. Under optimal conditions of stimulation, ICOS but not CD28 costimulation can be prevented by PD-1 engagement. IL-2 levels induced by costimulation are critical in determining the outcome of the PD-1 engagement. Thus, low to marginal IL-2 levels produced upon ICOS costimulation account for the greater sensitivity of this pathway to PD-1-mediated inhibition. Interestingly, exogenous IL-2, IL-7, and IL-15 but not IL-4 and IL-21 can rescue PD-1 inhibition, suggesting that among these cytokines only those that activate STAT5 can rescue PD-1 inhibition. As STAT5 has been implicated in the maintenance of IL-2Ralpha expression, these results suggest that IL-7 and IL-15 restore proliferation under conditions of PD-1 engagement by enhancing high-affinity IL-2R expression and hence, IL-2 responsiveness.