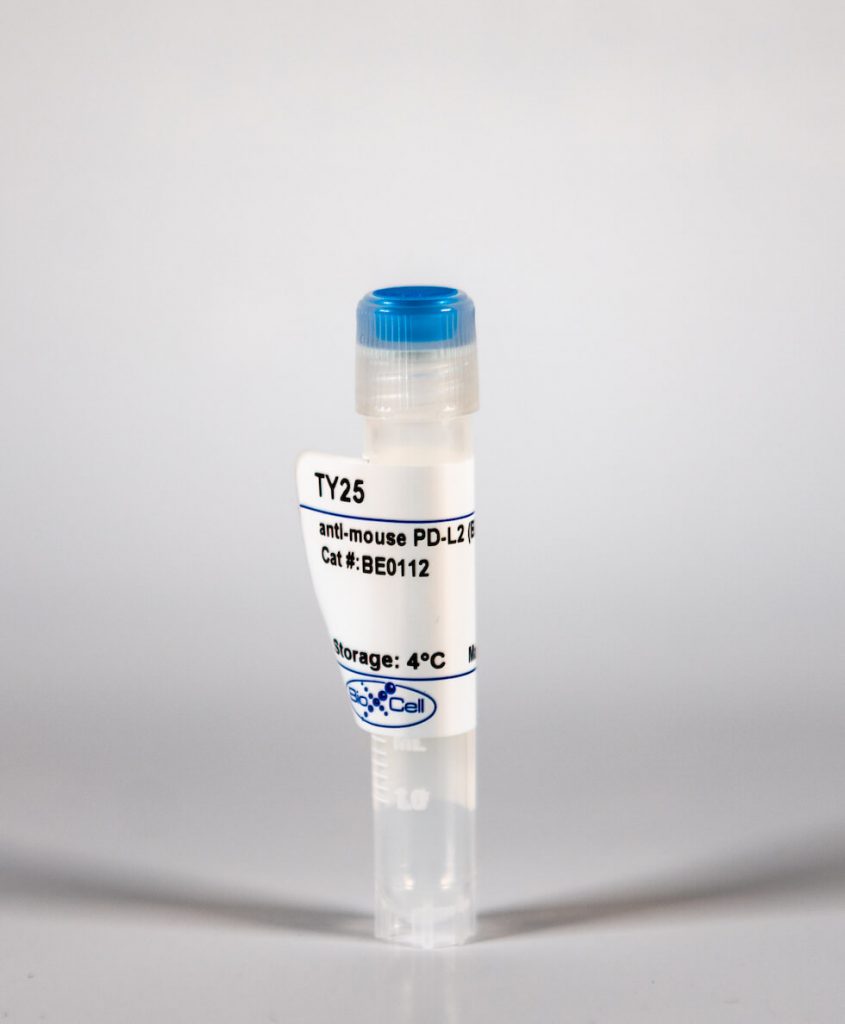
InVivoMab anti-mouse PD-L2 (B7-DC)
| Clone | TY25 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Catalog # | BE0112 | ||||||||||||
| Category | InVivoMab Antibodies | ||||||||||||
| Price |
|
The TY25 monoclonal antibody reacts with mouse PD-L2 (programmed death ligand 2) also known as B7-DC or CD273. PD-L2 is a 25 kDa type I transmembrane protein that belongs to the B7 family of the Ig superfamily. PD-L2 is expressed on monocytes, macrophages and subsets of dendritic cells. PD-L2 binds to its receptor, PD-1, found on CD4 and CD8 thymocytes as well as activated T and B lymphocytes and myeloid cells. Engagement of PD-L2 with PD-1 leads to inhibition of TCR-mediated T cell proliferation and cytokine production. The TY25 antibody has been reported to block PD-1 mediated interactions in vivo.
| Isotype | Rat IgG2a, κ |
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure™ pH 7.0 Dilution Buffer |
| Immunogen | Mouse PD-L2 transfected cell line |
| Reported Applications |
|
| Formulation |
|
| Endotoxin |
|
| Purity |
|
| Sterility | 0.2 μM filtered |
| Production | Purified from tissue culture supernatant in an animal free facility |
| Purification | Protein G |
| RRID | AB_10950106 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
InVivoMAb anti-mouse PD-L2 (B7-DC) (Clone: TY25)
Jaworska, K., et al. (2015). “Both PD-1 ligands protect the kidney from ischemia reperfusion injury.” J Immunol 194(1): 325-333. PubMed
Acute kidney injury (AKI) is a common problem in hospitalized patients that enhances morbidity and mortality and promotes the development of chronic and end-stage renal disease. Ischemia reperfusion injury (IRI) is one of the major causes of AKI and is characterized by uncontrolled renal inflammation and tubular epithelial cell death. Our recent studies demonstrated that regulatory T cells (Tregs) protect the kidney from ischemia reperfusion-induced inflammation and injury. Blockade of programmed death-1 (PD-1) on the surface of Tregs, prior to adoptive transfer, negates their ability to protect against ischemic kidney injury. The present study was designed to investigate the role of the known PD-1 ligands, PD-L1 and PD-L2, in kidney IRI. Administration of PD-L1 or PD-L2 blocking Abs prior to mild or moderate kidney IRI significantly exacerbated the loss of renal function, renal inflammation, and acute tubular necrosis compared with mice receiving isotype control Abs. Interestingly, blockade of both PD-1 ligands resulted in worse injury, dysfunction, and inflammation than did blocking either ligand alone. Genetic deficiency of either PD-1 ligand also exacerbated kidney dysfunction and acute tubular necrosis after subthreshold ischemia. Bone marrow chimeric studies revealed that PD-L1 expressed on non-bone marrow-derived cells is critical for this resistance to IRI. Finally, blockade of either PD-1 ligand negated the protective ability of adoptively transferred Tregs in IRI. These findings suggest that PD-L1 and PD-L2 are nonredundant aspects of the natural protective response to ischemic injury and may be novel therapeutic targets for AKI.
McKay, J. T., et al. (2015). “PD-1 suppresses protective immunity to Streptococcus pneumoniae through a B cell-intrinsic mechanism.” J Immunol 194(5): 2289-2299. PubMed
Despite the emergence of the programmed cell death 1 (PD-1):PD-1 ligand (PD-L) regulatory axis as a promising target for treating multiple human diseases, remarkably little is known about how this pathway regulates responses to extracellular bacterial infections. We found that PD-1(-/-) mice, as well as wild-type mice treated with a PD-1 blocking Ab, exhibited significantly increased survival against lethal Streptococcus pneumoniae infection following either priming with low-dose pneumococcal respiratory infection or S. pneumoniae-capsular polysaccharide immunization. Enhanced survival in mice with disrupted PD-1:PD-L interactions was explained by significantly increased proliferation, isotype switching, and IgG production by pneumococcal capsule-specific B cells. Both PD-L, B7-H1 and B7-DC, contributed to PD-1-mediated suppression of protective capsule-specific IgG. Importantly, PD-1 was induced on capsule-specific B cells and suppressed IgG production and protection against pneumococcal infection in a B cell-intrinsic manner. To our knowledge, these results provide the first demonstration of a physiologic role for B cell-intrinsic PD-1 expression in vivo. In summary, our study reveals that B cell-expressed PD-1 plays a central role in regulating protection against S. pneumoniae, and thereby represents a promising target for bolstering immunity to encapsulated bacteria.
Tkachev, V., et al. (2015). “Programmed death-1 controls T cell survival by regulating oxidative metabolism.” J Immunol 194(12): 5789-5800. PubMed
The coinhibitory receptor programmed death-1 (PD-1) maintains immune homeostasis by negatively regulating T cell function and survival. Blockade of PD-1 increases the severity of graft-versus-host disease (GVHD), but the interplay between PD-1 inhibition and T cell metabolism is not well studied. We found that both murine and human alloreactive T cells concomitantly upregulated PD-1 expression and increased levels of reactive oxygen species (ROS) following allogeneic bone marrow transplantation. This PD-1(Hi)ROS(Hi) phenotype was specific to alloreactive T cells and was not observed in syngeneic T cells during homeostatic proliferation. Blockade of PD-1 signaling decreased both mitochondrial H2O2 and total cellular ROS levels, and PD-1-driven increases in ROS were dependent upon the oxidation of fatty acids, because treatment with etomoxir nullified changes in ROS levels following PD-1 blockade. Downstream of PD-1, elevated ROS levels impaired T cell survival in a process reversed by antioxidants. Furthermore, PD-1-driven changes in ROS were fundamental to establishing a cell’s susceptibility to subsequent metabolic inhibition, because blockade of PD-1 decreased the efficacy of later F1F0-ATP synthase modulation. These data indicate that PD-1 facilitates apoptosis in alloreactive T cells by increasing ROS in a process dependent upon the oxidation of fat. In addition, blockade of PD-1 undermines the potential for subsequent metabolic inhibition, an important consideration given the increasing use of anti-PD-1 therapies in the clinic.
Erickson, J. J., et al. (2014). “Programmed death-1 impairs secondary effector lung CD8(+) T cells during respiratory virus reinfection.” J Immunol 193(10): 5108-5117. PubMed
Reinfections with respiratory viruses are common and cause significant clinical illness, yet precise mechanisms governing this susceptibility are ill defined. Lung Ag-specific CD8(+) T cells (T(CD8)) are impaired during acute viral lower respiratory infection by the inhibitory receptor programmed death-1 (PD-1). To determine whether PD-1 contributes to recurrent infection, we first established a model of reinfection by challenging B cell-deficient mice with human metapneumovirus (HMPV) several weeks after primary infection, and found that HMPV replicated to high titers in the lungs. A robust secondary effector lung TCD8 response was generated during reinfection, but these cells were more impaired and more highly expressed the inhibitory receptors PD-1, LAG-3, and 2B4 than primary T(CD8). In vitro blockade demonstrated that PD-1 was the dominant inhibitory receptor early after reinfection. In vivo therapeutic PD-1 blockade during HMPV reinfection restored lung T(CD8) effector functions (i.e., degranulation and cytokine production) and enhanced viral clearance. PD-1 also limited the protective efficacy of HMPV epitope-specific peptide vaccination and impaired lung T(CD8) during heterotypic influenza virus challenge infection. Our results indicate that PD-1 signaling may contribute to respiratory virus reinfection and evasion of vaccine-elicited immune responses. These results have important implications for the design of effective vaccines against respiratory viruses.
Jensen, K. D., et al. (2013). “Toxoplasma gondii rhoptry 16 kinase promotes host resistance to oral infection and intestinal inflammation only in the context of the dense granule protein GRA15.” Infect Immun 81(6): 2156-2167. PubMed
Toxoplasma gondii transmission between intermediate hosts is dependent on the ingestion of walled cysts formed during the chronic phase of infection. Immediately following consumption, the parasite must ensure survival of the host by preventing adverse inflammatory responses and/or by limiting its own replication. Since the Toxoplasma secreted effectors rhoptry 16 kinase (ROP16) and dense granule 15 (GRA15) activate the JAK-STAT3/6 and NF-kappaB signaling pathways, respectively, we explored whether a particular combination of these effectors impacted intestinal inflammation and parasite survival in vivo. Here we report that expression of the STAT-activating version of ROP16 in the type II strain (strain II+ROP16I) promotes host resistance to oral infection only in the context of endogenous GRA15 expression. Protection was characterized by a lower intestinal parasite burden and dampened inflammation. Host resistance to the II+ROP16I strain occurred independently of STAT6 and the T cell coinhibitory receptors B7-DC and B7-H1, two receptors that are upregulated by ROP16. In addition, coexpression of ROP16 and GRA15 enhanced parasite susceptibility within tumor necrosis factor alpha/gamma interferon-stimulated macrophages in a STAT3/6-independent manner. Transcriptional profiling of infected STAT3- and STAT6-deficient macrophages and parasitized Peyer’s patches from mice orally challenged with strain II+ROP16I suggested that ROP16 activated STAT5 to modulate host gene expression. Consistent with this supposition, the ROP16 kinase induced the sustained phosphorylation and nuclear localization of STAT5 in Toxoplasma-infected cells. In summary, only the combined expression of both GRA15 and ROP16 promoted host resistance to acute oral infection, and Toxoplasma may possibly target the STAT5 signaling pathway to generate protective immunity in the gut.
van der Werf, N., et al. (2013). “Th2 cell-intrinsic hypo-responsiveness determines susceptibility to helminth infection.” PLoS Pathog 9(3): e1003215. PubMed
The suppression of protective Type 2 immunity is a principal factor driving the chronicity of helminth infections, and has been attributed to a range of Th2 cell-extrinsic immune-regulators. However, the intrinsic fate of parasite-specific Th2 cells within a chronic immune down-regulatory environment, and the resultant impact such fate changes may have on host resistance is unknown. We used IL-4gfp reporter mice to demonstrate that during chronic helminth infection with the filarial nematode Litomosoides sigmodontis, CD4(+) Th2 cells are conditioned towards an intrinsically hypo-responsive phenotype, characterised by a loss of functional ability to proliferate and produce the cytokines IL-4, IL-5 and IL-2. Th2 cell hypo-responsiveness was a key element determining susceptibility to L. sigmodontis infection, and could be reversed in vivo by blockade of PD-1 resulting in long-term recovery of Th2 cell functional quality and enhanced resistance. Contrasting with T cell dysfunction in Type 1 settings, the control of Th2 cell hypo-responsiveness by PD-1 was mediated through PD-L2, and not PD-L1. Thus, intrinsic changes in Th2 cell quality leading to a functionally hypo-responsive phenotype play a key role in determining susceptibility to filarial infection, and the therapeutic manipulation of Th2 cell-intrinsic quality provides a potential avenue for promoting resistance to helminths.
Hafalla, J. C., et al. (2012). “The CTLA-4 and PD-1/PD-L1 inhibitory pathways independently regulate host resistance to Plasmodium-induced acute immune pathology.” PLoS Pathog 8(2): e1002504. PubMed
The balance between pro-inflammatory and regulatory immune responses in determining optimal T cell activation is vital for the successful resolution of microbial infections. This balance is maintained in part by the negative regulators of T cell activation, CTLA-4 and PD-1/PD-L, which dampen effector responses during chronic infections. However, their role in acute infections, such as malaria, remains less clear. In this study, we determined the contribution of CTLA-4 and PD-1/PD-L to the regulation of T cell responses during Plasmodium berghei ANKA (PbA)-induced experimental cerebral malaria (ECM) in susceptible (C57BL/6) and resistant (BALB/c) mice. We found that the expression of CTLA-4 and PD-1 on T cells correlates with the extent of pro-inflammatory responses induced during PbA infection, being higher in C57BL/6 than in BALB/c mice. Thus, ECM develops despite high levels of expression of these inhibitory receptors. However, antibody-mediated blockade of either the CTLA-4 or PD-1/PD-L1, but not the PD-1/PD-L2, pathways during PbA-infection in ECM-resistant BALB/c mice resulted in higher levels of T cell activation, enhanced IFN-gamma production, increased intravascular arrest of both parasitised erythrocytes and CD8(+) T cells to the brain, and augmented incidence of ECM. Thus, in ECM-resistant BALB/c mice, CTLA-4 and PD-1/PD-L1 represent essential, independent and non-redundant pathways for maintaining T cell homeostasis during a virulent malaria infection. Moreover, neutralisation of IFN-gamma or depletion of CD8(+) T cells during PbA infection was shown to reverse the pathologic effects of regulatory pathway blockade, highlighting that the aetiology of ECM in the BALB/c mice is similar to that in C57BL/6 mice. In summary, our results underscore the differential and complex regulation that governs immune responses to malaria parasites.
Huber, S., et al. (2010). “Alternatively activated macrophages inhibit T-cell proliferation by Stat6-dependent expression of PD-L2.” Blood 116(17): 3311-3320. PubMed
Alternatively activated macrophages (AAM) accumulate in tissues during Th2-associated immune responses like helminth infections and allergic disorders. These cells differentiate in response to interleukin 4 (IL-4)/IL-13-mediated activation of Stat6 and possess potent inhibitory activity against T cells. The molecular mechanism that leads to T-cell suppression remains unclear and could involve soluble factors or inhibitory ligands. Microarray analysis revealed that the inhibitory ligand, programmed death ligand 2 (PD-L2) was strongly induced by IL-4 in macrophages from wild-type but not Stat6-deficient mice. PD-L2 expression correlated with other established markers for AAM-like Relm-alpha/Fizz1, arginase1, or Ym1 and thereby serves as useful surface marker to identify and isolate AAM from tissues. Antibodies against PD-L2 blocked the inhibitory activity of AAM and retroviral expression of PD-L2 in macrophages from Stat6(-/-) mice was sufficient to inhibit T-cell proliferation, which demonstrates that PD-L2 mediates potent and nonredundant inhibition of T cells independently of other Stat6-regulated genes. Infection of conditional IL-4/IL-13-deficient mice with the helminth Nippostrongylus brasiliensis further showed that PD-L2 expression was dependent on IL-4/IL-13 from Th2 cells. In vivo blockade of PD-L2 during N brasiliensis infection caused an enhanced Th2 response in the lung, indicating that AAM inhibit Th2 cells by expression of PD-L2.