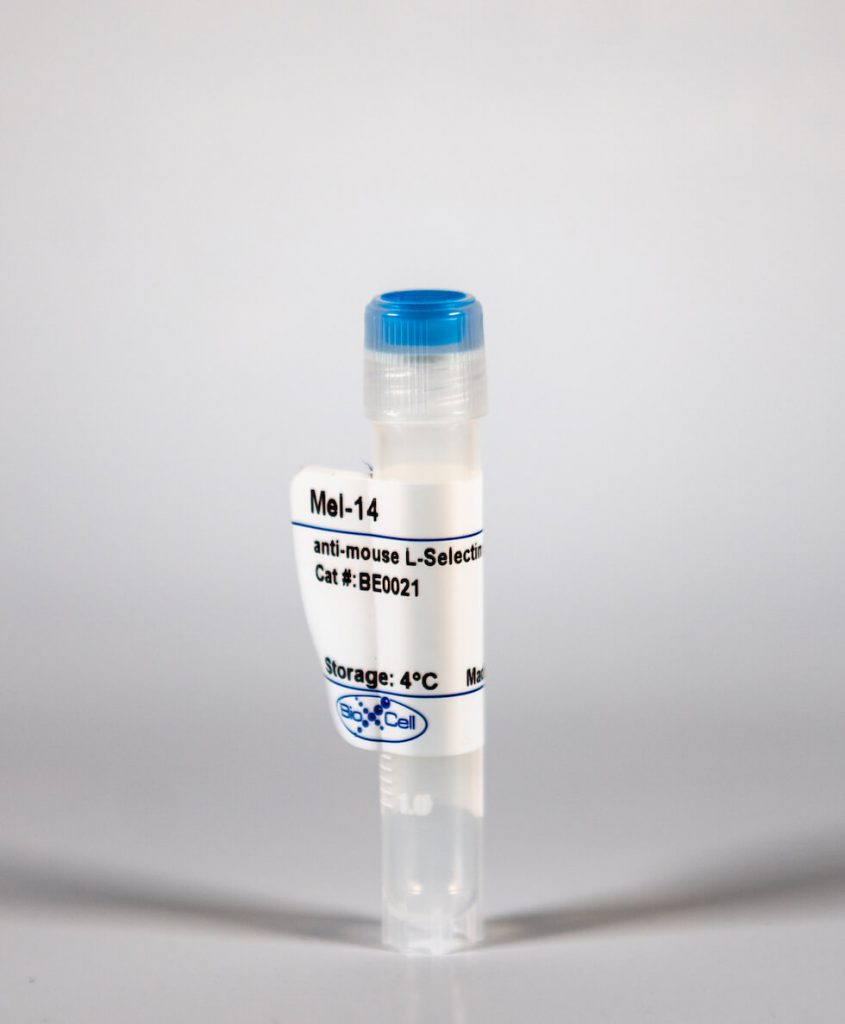
InVivoMAb anti-mouse L-Selectin (CD62L)
| Clone | Mel-14 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Catalog # | BE0021 | ||||||||||||
| Category | InVivoMab Antibodies | ||||||||||||
| Price |
|
The Mel-14 monoclonal antibody reacts with mouse CD62L also known as L-selectin and MEL-14. CD62L is a 76 kDa glycoprotein and a member of the selectin family that is expressed by neutrophils, monocytes, the majority of naïve T and B cells, a subset of memory T cells, NK cells, and most thymocytes. CD62L is a cell adhesion molecule that binds to many glycoprotein ligands including CD34, GlyCAM-1, MAdCAM-1, and PSGL-1 and acts as a "homing receptor" for lymphocytes to enter secondary lymphoid tissues via high endothelial venules.The Mel-14 monoclonal antibody reacts with mouse CD62L also known as L-selectin and MEL-14. CD62L is a 76 kDa glycoprotein and a member of the selectin family that is expressed by neutrophils, monocytes, the majority of naïve T and B cells, a subset of memory T cells, NK cells, and most thymocytes. CD62L is a cell adhesion molecule that binds to many glycoprotein ligands including CD34, GlyCAM-1, MAdCAM-1, and PSGL-1 and acts as a "homing receptor" for lymphocytes to enter secondary lymphoid tissues via high endothelial venules.
| Isotype | Rat IgG2a, κ |
| Recommended Isotype Control(s) | InVivoMAb rat IgG2a isotype control, anti-trinitrophenol |
| Recommended Dilution Buffer | InVivoPure™ pH 7.0 Dilution Buffer |
| Immunogen | C3H/eb mouse B lymphoma 38C-13 |
| Reported Applications | in vivo CD62L neutralization |
| Formulation |
|
| Endotoxin |
|
| Purity |
|
| Sterility | 0.2 μM filtered |
| Production | Purified from tissue culture supernatant in an animal free facility |
| Purification | Protein G |
| RRID | AB_1107665 |
| Molecular Weight | 150 kDa |
| Storage | The antibody solution should be stored at the stock concentration at 4°C. Do not freeze. |
INVIVOMAB ANTI-MOUSE L-SELECTIN (CD62L) (CLONE: MEL-14)
Brinkman, C. C., et al. (2016). “Treg engage lymphotoxin beta receptor for afferent lymphatic transendothelial migration.” Nat Commun 7: 12021. PubMed
Regulatory T cells (Tregs) are essential to suppress unwanted immunity or inflammation. After islet allo-transplant Tregs must migrate from blood to allograft, then via afferent lymphatics to draining LN to protect allografts. Here we show that Tregs but not non-Treg T cells use lymphotoxin (LT) during migration from allograft to draining LN, and that LT deficiency or blockade prevents normal migration and allograft protection. Treg LTalphabeta rapidly modulates cytoskeletal and membrane structure of lymphatic endothelial cells; dependent on VCAM-1 and non-canonical NFkappaB signalling via LTbetaR. These results demonstrate a form of T-cell migration used only by Treg in tissues that serves an important role in their suppressive function and is a unique therapeutic focus for modulating suppression.
Guidotti, L. G., et al. (2015). “Immunosurveillance of the liver by intravascular effector CD8(+) T cells.” Cell 161(3): 486-500. PubMed
Effector CD8(+) T cells (CD8 TE) play a key role during hepatotropic viral infections. Here, we used advanced imaging in mouse models of hepatitis B virus (HBV) pathogenesis to understand the mechanisms whereby these cells home to the liver, recognize antigens, and deploy effector functions. We show that circulating CD8 TE arrest within liver sinusoids by docking onto platelets previously adhered to sinusoidal hyaluronan via CD44. After the initial arrest, CD8 TE actively crawl along liver sinusoids and probe sub-sinusoidal hepatocytes for the presence of antigens by extending cytoplasmic protrusions through endothelial fenestrae. Hepatocellular antigen recognition triggers effector functions in a diapedesis-independent manner and is inhibited by the processes of sinusoidal defenestration and capillarization that characterize liver fibrosis. These findings reveal the dynamic behavior whereby CD8 TE control hepatotropic pathogens and suggest how liver fibrosis might reduce CD8 TE immune surveillance toward infected or transformed hepatocytes.
Cremasco, V., et al. (2014). “B cell homeostasis and follicle confines are governed by fibroblastic reticular cells.” Nat Immunol 15(10): 973-981. PubMed
Fibroblastic reticular cells (FRCs) are known to inhabit T cell-rich areas of lymphoid organs, where they function to facilitate interactions between T cells and dendritic cells. However, in vivo manipulation of FRCs has been limited by a dearth of genetic tools that target this lineage. Here, using a mouse model to conditionally ablate FRCs, we demonstrated their indispensable role in antiviral T cell responses. Unexpectedly, loss of FRCs also attenuated humoral immunity due to impaired B cell viability and follicular organization. Follicle-resident FRCs established a favorable niche for B lymphocytes via production of the cytokine BAFF. Thus, our study indicates that adaptive immunity requires an intact FRC network and identifies a subset of FRCs that control B cell homeostasis and follicle identity.
Harp, J. R., et al. (2010). “Memory T cells are enriched in lymph nodes of selectin-ligand-deficient mice.” J Immunol 185(10): 5751-5761. PubMed
Fucosyltransferase-IV and -VII double knockout (FtDKO) mice reveal profound impairment in T cell trafficking to lymph nodes (LNs) due to an inability to synthesize selectin ligands. We observed an increase in the proportion of memory/effector (CD44(high)) T cells in LNs of FtDKO mice. We infected FtDKO mice with lymphocytic choriomeningitis virus to generate and track Ag-specific CD44(high)CD8 T cells in secondary lymphoid organs. Although frequencies were similar, total Ag-specific effector CD44(high)CD8 T cells were significantly reduced in LNs, but not blood, of FtDKO mice at day 8. In contrast, frequencies of Ag-specific memory CD44(high)CD8 T cells were up to 8-fold higher in LNs of FtDKO mice at day 60. Because wild-type mice treated with anti-CD62L treatment also showed increased frequencies of CD44(high) T cells in LNs, we hypothesized that memory T cells were preferentially retained in, or preferentially migrated to, FtDKO LNs. We analyzed T cell entry and egress in LNs using adoptive transfer of bone fide naive or memory T cells. Memory T cells were not retained longer in LNs compared with naive T cells; however, T cell exit slowed significantly as T cell numbers declined. Memory T cells were profoundly impaired in entering LNs of FtDKO mice; however, memory T cells exhibited greater homeostatic proliferation in FtDKO mice. These results suggest that memory T cells are enriched in LNs with T cell deficits by several mechanisms, including longer T cell retention and increased homeostatic proliferation.
Harp, J. R. and T. M. Onami (2010). “Naive T cells re-distribute to the lungs of selectin ligand deficient mice.” PLoS One 5(6): e10973. PubMed
BACKGROUND: Selectin mediated tethering represents one of the earliest steps in T cell extravasation into lymph nodes via high endothelial venules and is dependent on the biosynthesis of sialyl Lewis X (sLe(x)) ligands by several glycosyltransferases, including two fucosyltransferases, fucosyltransferase-IV and -VII. Selectin mediated binding also plays a key role in T cell entry to inflamed organs. METHODOLOGY/PRINCIPAL FINDINGS: To understand how loss of selectin ligands (sLe(x)) influences T cell migration to the lung, we examined fucosyltransferase-IV and -VII double knockout (FtDKO) mice. We discovered that FtDKO mice showed significant increases (approximately 5-fold) in numbers of naive T cells in non-inflamed lung parenchyma with no evidence of induced bronchus-associated lymphoid tissue. In contrast, activated T cells were reduced in inflamed lungs of FtDKO mice following viral infection, consistent with the established role of selectin mediated T cell extravasation into inflamed lung. Adoptive transfer of T cells into FtDKO mice revealed impaired T cell entry to lymph nodes, but selective accumulation in non-lymphoid organs. Moreover, inhibition of T cell entry to the lymph nodes by blockade of L-selectin, or treatment of T cells with pertussis toxin to inhibit chemokine dependent G-coupled receptor signaling, also resulted in increased T cells in non-lymphoid organs. Conversely, inhibition of T cell egress from lymph nodes using FTY720 agonism of S1P1 impaired T cell migration into non-lymphoid organs. CONCLUSIONS/SIGNIFICANCE: Taken together, our results suggest that impaired T cell entry into lymph nodes via high endothelial venules due to genetic deficiency of selectin ligands results in the selective re-distribution and accumulation of T cells in non-lymphoid organs, and correlates with their increased frequency in the blood. Re-distribution of T cells into organs could potentially play a role in the initiation of T cell mediated organ diseases.